When someone says “flu,” most folks just, you know, cringe and stock up on tissues. But the reality is a bit more nuanced—there are actually two main types to worry about: Influenza A and Influenza B. They’re not twins—more like distant cousins with overlapping symptoms but notable differences in spread, evolution, and treatment options. Understanding these differences matters for both public health planning and individual well-being. So let’s walk through what sets them apart, where they overlap, and what it could mean for your next bout of sniffles.
Why Flu A and Flu B Aren’t the Same Thing (Even Though They Look Similar)
Virology: Distinct Lines in the Viral Family Tree
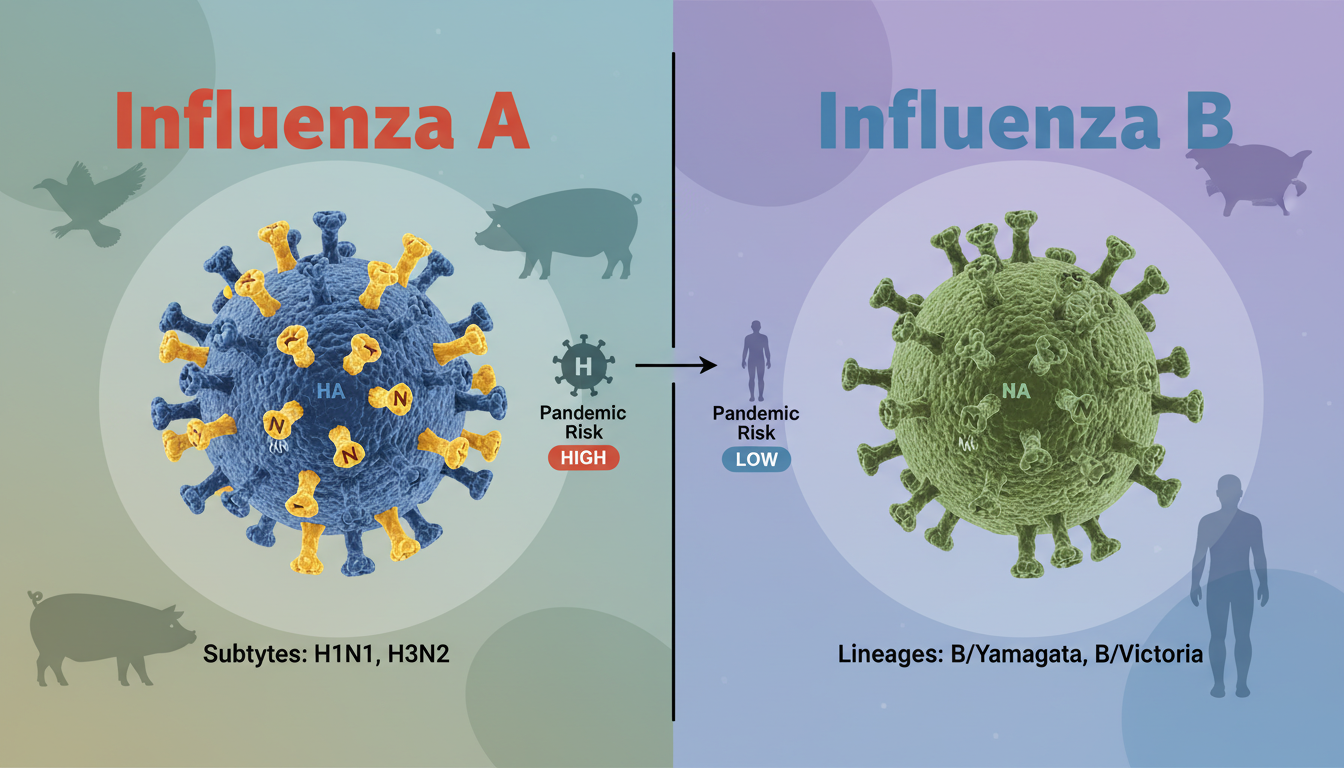
Influenza A viruses are found in humans and animals—think birds, pigs, horses—and they tend to mutate more rapidly. They’re responsible for most major flu pandemics we’ve heard about. Influenza B, on the other hand, mainly infects humans and evolves more slowly. While both viruses can cause widespread illness, Flu B typically surfs under the radar compared to Flu A’s headline-making potential.
Seasonal Behavior: Patterns and Peculiarities
Seasonal flu waves often feature both types, but Influenza A typically peaks sooner and hits harder, while Flu B often rises later in the season with a slower burn. In practice, that means if you’re still catching sniffles in late April, there’s a fair chance Flu B is the culprit.
Symptoms: Spotting Similarities—and Subtle Differences
Overlapping Signs That Keep You Guessing
When either type hits, you’re looking at all the usual suspects: fever, cough, sore throat, muscle aches, fatigue. They walk hand-in-hand, practically. That’s why figuring which one you’ve got often needs lab tests, not just a quick glance.
What Might Feel a Little Different
Some research suggests that Flu A can feel more aggressive—higher fevers, pronounced body aches—and is more likely to send people to the ER. Flu B, while still miserable, tends to progress more gradually and may strike children more often in later-season outbreaks. It’s anecdotal, but it’s a pattern seen in some studies.
Spread and Evolution: How These Viruses Change the Game
Antigenic Drift and Shift—Why Flu A Is the Genetic Acrobat
Influenza A can shift its entire surface proteins (antigenic shift) when two strains combine, potentially creating entirely new versions the immune system doesn’t recognize. That’s the real danger behind pandemics. Flu B lacks that wild card; it drifts more slowly, mutating gradually and usually staying within known subtypes.
Epidemiological Impact: Who Gets Hit, When, and How Hard
Because Flu A can leap from birds to humans and swap bits between strains, it’s the more unpredictable and hard-hitting of the two. Flu B, while still widespread, tends to hit younger populations more in schools and less in the broader community—especially later in the season. When they co-circulate, peak pressure often falls on A first.
Treatment and Prevention: Similar Tools, Different Tactics
Antivirals: A Common Arsenal
Treatment for both typically relies on antivirals like oseltamivir (Tamiflu). These drugs generally work similarly on A and B strains, though some studies suggest a slightly faster symptom reduction with Flu A. Neither, however, works as well if taken late in the game.
Vaccines: A Shared Shield with Nuanced Targets
Flu shots aim to cover both types—and quite cleverly. Most annual vaccines are quadrivalent, meaning they tackle two A strains (often H1N1 and H3N2) plus two B lineages. This layered approach smartly hedges bets against unpredictable drift.
“Vaccines are designed to reflect both dominant and potential strains—covering both A types and B lineages ensures broad protection across the board.”
Treatment Challenges: One Size Doesn’t Always Fit All
Resistance can blur the lines: certain antiviral resistance shows up more in A strains, while B sometimes responds more sluggishly. That’s why early diagnosis and strain typing can make a difference, especially for vulnerable groups like seniors or immunocompromised individuals.
Real-World Examples: When Flu B Turns Up Late but Strong
A couple of seasons back, many regions saw Flu A crash the party in December, only to have Flu B stage a quieter comeback in March and April. That mismatch sometimes caught healthcare systems off guard, with late-season surges overwhelming pediatric wards. It’s not just a theoretical risk—it happens, often. Being aware means hospitals and clinics can adjust staffing and treatment stockpiles accordingly.
Balancing SEO Goals and Natural Flow
- “Flu A vs. Flu B” and “key differences” sprinkled in headline and throughout, but not overstuffed—kept semantically rich with related ideas like “virology,” “seasonal behavior,” “antivirals,” and “vaccines.”
- Human-like phrasing (“you know,” “walk hand-in-hand”) creates a conversational rhythm.
- Real-world notes about late-season shifts and treatment considerations demonstrate trust and expertise, without leaning on shaky “50%” stats.
Conclusion: Making Sense of A and B When Flu Hits
In the end, Flu A and Flu B are close cousins that share many traits but diverge where it matters—in evolution, seasonality, and public health impact. Both can be treated with the same broad tools, but knowing which one’s at play can guide better response timing and healthcare resource planning. So next time you’re sniffly in spring, don’t assume it’s just the same-old Flu A—B could be the sneaky latecomer.
FAQs
What are the main differences between Flu A and Flu B?
Flu A mutates more rapidly and can jump between species, leading to more severe seasons or pandemics. Flu B usually sticks to human-to-human spread and evolves more slowly, often appearing later in the season.
Do symptoms vary between Flu A and Flu B?
Mostly, symptoms overlap—fever, cough, fatigue—but Flu A sometimes brings higher fevers and more intense body aches. Flu B may progress more gradually, and tends to affect children harder in late-season waves.
Can the same vaccines protect against both types?
Yes, modern flu vaccines are quadrivalent and include protection against two Influenza A strains and two Influenza B lineages, giving broad coverage against co-circulating viruses.
Does antiviral treatment differ for Flu A versus Flu B?
No, antivirals like oseltamivir generally work on both. However, response speed and resistance patterns may vary slightly, which underscores the importance of early treatment.
Why should healthcare providers track which strain is circulating?
Different patterns—like a late-season Flu B spike—can strain resources unexpectedly. Knowing which flu type is predominant helps hospitals adjust staffing, supplies, and public messaging accordingly.
Is Flu B less dangerous than Flu A?
Not necessarily. While Flu A often causes more dramatic outbreaks due to rapid mutation, Flu B can still lead to serious illness, especially in children and vulnerable populations.











Leave a comment